
Emerging

Emerging
CAR T Cancer Treatment Gets A Boost
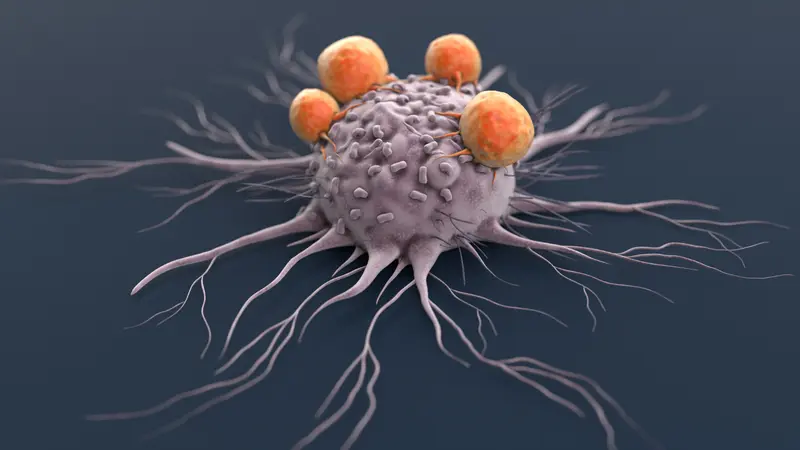
CAR T cell therapy, first approved by the U.S. Food and Drug Administration in 2017, is a cutting-edge cancer treatment that reprograms a patient’s own immune cells, called T cells, to better recognize and destroy cancer cells.
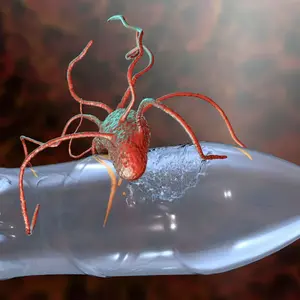
The treatment involves collecting a blood sample from a patient and extracting T cells that are sent to a lab to be enhanced. The T cells are engineered to produce a special protein on their surface known as a chimeric antigen receptor (CAR). The modified T cells are infused back into the patient’s bloodstream. The receptor guides the T cell to find and attack cancer cells with matching markers.
CAR T therapy has saved many lives, especially for blood cancers like leukemia and lymphoma, but the treatment does not always last. Over time, the modified T cells can become exhausted, die off, or lose their ability to recognize cancer, a problem known as CAR T cell dysfunction.
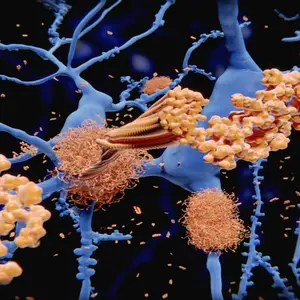
To solve this problem, researchers have been experimenting with improving the tools used to modify the T cells. In some emerging clinical trials, T cells are changed using CRISPR, a powerful gene-editing technology that acts like molecular scissors to precisely “knock out” (turn off) individual genes and observe how that change influences the cell’s behavior.
To further improve the CRISPR technology, scientists built a new experimental research system called CELLFIE. Using CELLFIE, scientists systematically turned off nearly every gene in human CAR T cells to find out which ones help or hinder their cancer-fighting abilities. They then measured how these genetic edits affected key features of T cell biology, such as how well the cells multiplied, recognized targets, activated immune responses, mistakeningly attacked each other, or became exhausted over time. This new technology improved the scale and speed of the bioengineering process, allowing scientists to test almost every gene in the T cells and measure key aspects of their biology.
In tests on mice with leukemia, the researchers discovered that turning off a gene called RHOG made the CAR T cells significantly more effective at fighting cancer. When combining the RHOG knockout with a FAS knockout (a gene involved in triggering cell death), the enhanced CAR T cells were stronger and longer-lasting. These results were confirmed across different experimental models.
The CELLFIE platform provides a powerful new tool for improving cell-based immunotherapies, opening the door to more durable, precise and effective cancer treatments in the future. However, additional research and approvals are required before it can be used on human patients.
REFERENCES
Datlinger, P., Pankevich, E. V., Arnold, C. D., Pranckevicius, N., Lin, J., Romanovskaia, D., Schaefer, M., Piras, F., Orts, A.-C., Nemc, A., Biesaga, P. N., Chan, M., Neuwirth, T., Artemov, A. V., Li, W., Ladstätter, S., Krausgruber, T., & Bock, C. (2025). Systematic discovery of CRISPR-boosted CAR T cell immunotherapies. Nature, 646, 963–972. https://doi.org/10.1038/s41586-025-09507-9


 By
By