Complementary and Alternative Medicine (CAM)
Complementary and Alternative Medicine (CAM)
Transdermal Penetration Capabilities of Mesenchymal Stem Cell-Derived Extracellular Vesicles
by Sean Vandersluis, PhD and Adam Brockman, DC, ND
Topical therapies offer a highly attractive route of administration as it is non-invasive, bypasses first-pass metabolism, and convenient for patients, which can improve compliance. Yet, delivering biologics through the skin remains a major challenge. The stratum corneum, the skin’s outermost layer, is densely packed with lipids and keratin, forming a robust barrier that blocks most biologic agents.1
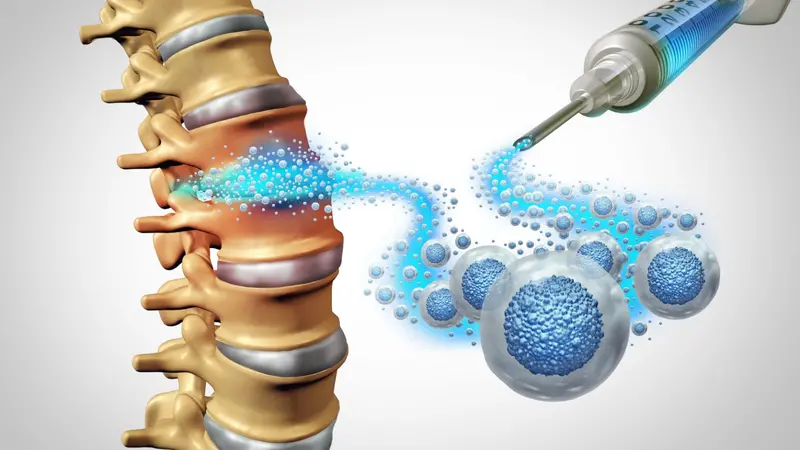
Mesenchymal stem cell-derived extracellular vesicles (MSC-EVs), offer a promising therapeutic approach to treat a number of dermatologic and musculoskeletal diseases. These nanoscale messengers, ranging from 30 to 150 nm, are naturally enclosed in a lipid bilayer and carry bioactive molecules like cytokines, growth factors, and lipids that promote tissue repair and modulate inflammation.2
Transdermal Penetration of MSC-EVs
On their own, MSC-EVs have limited transdermal penetration capabilities. Their lipid membranes can briefly loosen the stratum corneum’s lipid matrix, allowing small-scale passive diffusion through hair follicles3 and sweat glands4 , but only a fraction of vesicles reach deeper layers.5
Formulation strategies can improve delivery. Penetration enhancers like dimethyl sulfoxide (DMSO) and camphor are used in FDA-approved topical drugs for arthritis. DMSO is amphiphilic, disrupting lipid packing, altering keratin structure, and increasing hydration to create transient pathways.6 Camphor, a small lipophilic terpenoid, disrupts stratum corneum organization to boost permeability.7 Another approach is hybridization where MSC-EVs are coated or fused with synthetic lipid nanoparticles engineered for greater stability and skin penetration.8
Once inside the viable epidermis and dermis, MSC-EVs can deliver their bioactive cargo directly to local cells or be transported to deeper musculoskeletal tissues.9 This ability opens possibilities for non-invasive treatment of joint and tendon injuries, inflammatory arthropathies, and other connective tissue disorders.
Future Clinical Outlook
Topical MSC-EV therapies are gaining traction in clinical research. In a Phase 1 trial a topical MSC-EV formulation for psoriasis was well tolerated.10 Another study reported reduced melanin production in hyperpigmentation disorders.12 Preclinical research is exploring hydrogel embedding, and genetic engineering of parent cells to enhance vesicle stability and penetration.11 These continued advances open the door for effective MSC-EV based therapies for musculoskeletal diseases without the need for injections or invasive procedures.
This article first appeared in the November 2025 Issue of The American Chiropractor Magazine. Reprinted with permission.
REFERENCES
1. Matsui, T., and Amagai, M. (2015). Dissecting the formation, structure and barrier function of the stratum corneum. Int Immunol 27, 269–280. https://doi.org/10.1093/intimm/dxv013.
2. Maqsood, M., Kang, M., Wu, X., Chen, J., Teng, L., and Qiu, L. (2020). Adult mesenchymal stem cells and their exosomes: Sources, characteristics, and application in regenerative medicine. Life Sci 256, 118002. https://doi.org/10.1016/j.lfs.2020.118002.
3. Cheng, M., Ma, C., Chen, H.-D., Wu, Y., and Xu, X.-G. (2024). The Roles of Exosomes in Regulating Hair Follicle Growth. Clin Cosmet Investig Dermatol 17, 1603–1612. https://doi.org/10.2147/CCID.S465963.
4. Weng, T., Wu, P., Zhang, W., Zheng, Y., Li, Q., Jin, R., Chen, H., You, C., Guo, S., Han, C., et al. (2020). Regeneration of skin appendages and nerves: current status and further challenges. J Transl Med 18, 53. https://doi.org/10.1186/s12967-020-02248-5.
5. Yepes-Molina, L., Martínez-Ballesta, M.C., and Carvajal, M. (2020). Plant plasma membrane vesicles interaction with keratinocytes reveals their potential as carriers. J Adv Res 23, 101–111. https://doi.org/10.1016/j.jare.2020.02.004.
6. Marren, K. (2011). Dimethyl sulfoxide: an effective penetration enhancer for topical administration of NSAIDs. Phys Sportsmed 39, 75–82. https://doi.org/10.3810/psm.2011.09.1923.
7. Chen, J., Jiang, Q.D., Chai, Y.P., Zhang, H., Peng, P., and Yang, X.X. (2016). Natural terpenes as penetration enhancers for transdermal drug delivery. Preprint at MDPI AG, https://doi.org/10.3390/molecules21121709 https://doi.org/10.3390/molecules21121709.
8. Rodríguez, D.A., and Vader, P. (2022). Extracellular Vesicle-Based Hybrid Systems for Advanced Drug Delivery. Pharmaceutics 14. https://doi.org/10.3390/pharmaceutics14020267.
9. Mulcahy, L.A., Pink, R.C., and Carter, D.R.F. (2014). Routes and mechanisms of extracellular vesicle uptake. J Extracell Vesicles 3. https://doi.org/10.3402/jev.v3.24641.
10. Chandran, N.S., Bhupendrabhai, M.N., Tan, T.T., Zhang, B., Lim, S.K., Choo, A.B.H., and Lai, R.C. (2025). A phase 1, open-label study to determine safety and tolerability of the topical application of mesenchymal stem/stromal cell (MSC) exosome ointment to treat psoriasis in healthy volunteers. Cytotherapy 27, 633–641. https://doi.org/10.1016/j.jcyt.2025.01.007.
11. Bhat, A., Malik, A., Yadav, P., Ware, W.P.J., Kakalij, P., and Chand, S. (2024). Mesenchymal stem cell-derived extracellular vesicles: Recent therapeutics and targeted drug delivery advances. Preprint at John Wiley and Sons Inc, https://doi.org/10.1002/jex2.156 https://doi.org/10.1002/jex2.156.
12. Cho, B.S., Lee, J., Won, Y., Duncan, D.I., Jin, R.C., Lee, J., Kwon, H.H., Park, G.-H., Yang, S.H., Park, B.C., et al. (2020). Skin Brightening Efficacy of Exosomes Derived from Human Adipose Tissue-Derived Stem/Stromal Cells: A Prospective, Split-Face, Randomized Placebo-Controlled Study. Cosmetics 7, 90. https://doi.org/10.3390/cosmetics7040090.